What is Mpox?
Mpox (formerly known as monkeypox) is becoming a significant concern globally. You may be feeling uneasy about whether you need to protect yourself from the virus, especially with the rapid changes in vaccination guidelines. Are you unsure if the mpox vaccine is right for you in 2024? As vaccination efforts target various groups, it’s crucial to understand the facts. Should non-sexual individuals or healthcare professionals receive the vaccine? Let’s clarify the situation and examine the current recommendations, risk factors, and important details about the vaccine this year.
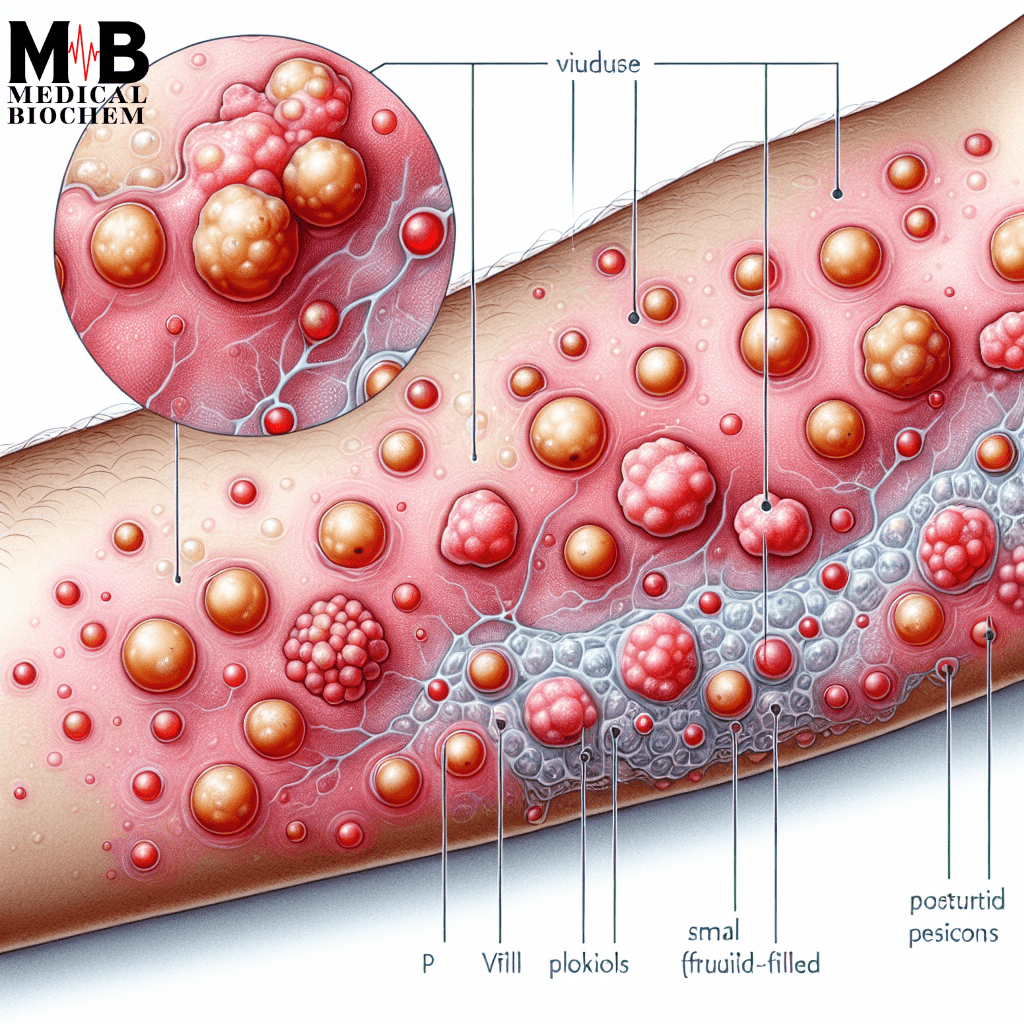
Mpox, a viral zoonotic disease, was once a rare infection mostly found in parts of central and West Africa. Recent outbreaks have expanded beyond their former regional scope. Human-to-human transmission, primarily through direct contact with infected skin, bodily fluids, or contaminated surfaces, has led to a rise in global cases. Symptoms include fever, rashes, swollen lymph nodes, and painful lesions that can last two to four weeks.
Why is the Mpox Vaccine Important?
The mpox vaccine plays a critical role in controlling outbreaks and preventing the further spread of the virus. The vaccine boosts your immune response to mpox. This makes it much less likely that you will experience severe symptoms if exposed to the virus. In 2024, health officials focused on high-risk groups and considered the changing dynamics of the virus.
Now that we understand what mpox is, let’s dive into who should consider getting the vaccine.
Who Should Get the Mpox Vaccine in 2024?
As of 2024, health authorities primarily recommended vaccinations against mpox for individuals in high-risk categories. While the virus can affect anyone, there are specific groups with a higher likelihood of exposure and serious infection. Understanding your risk level is key to deciding if you need the vaccine.
1. Doctors and Healthcare Workers
One of the most commonly asked questions is, “Do doctors get the mpox vaccine in 2024?” The answer depends largely on the nature of their work. Healthcare workers are at high risk of coming into contact with infectious diseases, especially those who work closely with skin or treat patients with viral infections.
Individuals handling mpox cases or those identified as high-risk should follow particular guidelines. Doctors are a priority group for vaccination because they are on the front lines, making them more susceptible to contracting and spreading the virus. The CDC and WHO have emphasized that even if healthcare workers are not in frequent contact with these patients, they should still evaluate their risk factors, particularly if their job involves exposure to bodily fluids.
2. Non-Sexual Individuals: Should You Get Vaccinated?
For non-sexual individuals, the risk may seem lower compared to those who are sexually active or frequently exposed to high-contact environments. For instance:
- If you live with someone at high risk, such as a healthcare worker or an immunocompromised person, getting the vaccine adds a layer of protection.
- If your job involves handling materials or working in environments of outbreak, consider getting vaccinated.
- For frequent travelers, in areas with higher mumps infection rates. For individuals and in these regions, getting is necessary.
Vaccination decisions are complex for non-sexual individuals. Experts advise assessing personal risk and potential exposure to make an informed choice.
How Does the Mpox Vaccine Work?
The mpox vaccine uses a weakened virus to stimulate the body’s immune system, enabling it to recognize and fight off the mpox virus if exposed. The most common mpox vaccine used is the JYNNEOS vaccine, which also protects against smallpox, due to the similarities between the two viruses.
JYNNEOS is a two-dose vaccine administered four weeks apart, ensuring that recipients have robust immunity. Most people can tolerate the vaccine well. Mild side effects, such as soreness at the injection site or a low-grade fever, may occur.
Why is the Vaccine Especially Important in 2024?
The 2024 guidelines for the mpox vaccine reflect a growing understanding of how the virus spreads and who is most at risk. Now, public health experts recognize that broader vaccination efforts may be necessary. Experts also advise that immunity from the vaccine may wane over time, leading to the possibility of booster shots in the coming years.
Addressing Common Concerns
1. Is the Vaccine Safe for Everyone?
The mpox vaccine is considered safe for most people, including individuals with weakened immune systems. However, it’s important to consult your healthcare provider if you have a history of severe allergies or adverse reactions to vaccines.
2. Does Vaccine Prevent All Mpox Cases?
No vaccine provides 100% protections, but the vaccine significantly reduces the risk of severe illness and hospitalization. Vaccinated people can still contact mpox. However, their symptoms are likely to be milder and less prolonged compared to those who are not vaccinated.
3. How Long Does the Vaccine Provide Protection?
Current data suggests that the vaccine provides protection for several years. However, as research continues, recommendations may shift towards booster doses, especially for those in high-risk categories.
Mpox and Public Perception
Since the mpox outbreak, concerns have arisen about who is eligible for the vaccine. Many people have expressed their concerns about the mpox vaccine recipients. They fear they may not fit the typical “at-risk” profile. It’s crucial to dispel myths around mpox. The virus is not exclusive to any one group, and anyone in close contact with an infected individual can catch it. Vaccination is not limited to sexually active individuals or healthcare workers. Everyone should assess their own exposure risks.
The 2024 vaccination strategy takes into account the shifting dynamics of the virus, and public health bodies are working hard to ensure that those who need it most can access the vaccine. Non-sexual individuals may not seem like an immediate priority for vaccination. However, they can still find value in getting vaccinated if certain circumstances warrant it.
Conclusion:
In 2024, the mpox vaccine continues to be a vital tool in curbing the spread of this virus. Whether you’re a doctor, healthcare worker, or simply trying to navigate your risk as a non-sexual person, it’s essential to stay informed. Doctors and healthcare workers are urged to get vaccinated, given their high exposure to potential infections. Non-sexual individuals should weigh their personal exposure risk, living situation, and professional environment to determine if vaccination is necessary.
The mpox vaccine is a critical measure to prevent outbreaks and protect the most vulnerable. As we move further into 2024, stay updated on the latest guidelines and make sure to consult your healthcare provider to make the best decision for your health.